Shoulder

Top Orthopaedic Shoulder Specialist In Portland
With its remarkable range of motion, the shoulder is a complicated and highly adaptable joint. However, every joint in the body has a trade-off between structural strength/stability and maneuverability. This means that in addition to being a very susceptible joint, the shoulder is also prone to inflammation and damage. This explains why, annually, shoulder pain affects approximately 18 million Americans. From the main ball-and-socket joint to the surrounding tendons and muscles, there are potentially numerous areas within the shoulder that may be the source of your discomfort. To address these issues, a correct diagnosis is necessary to identify the underlying cause and create a customized treatment plan for your illness. In this summary, we’ll look at some of the most frequent causes of shoulder discomfort, the anatomy involved, and how your doctor uses imaging studies, physical exam results, and your symptoms to effectively diagnose the issues

Rotator Cuff Specialist Near Portland, OR
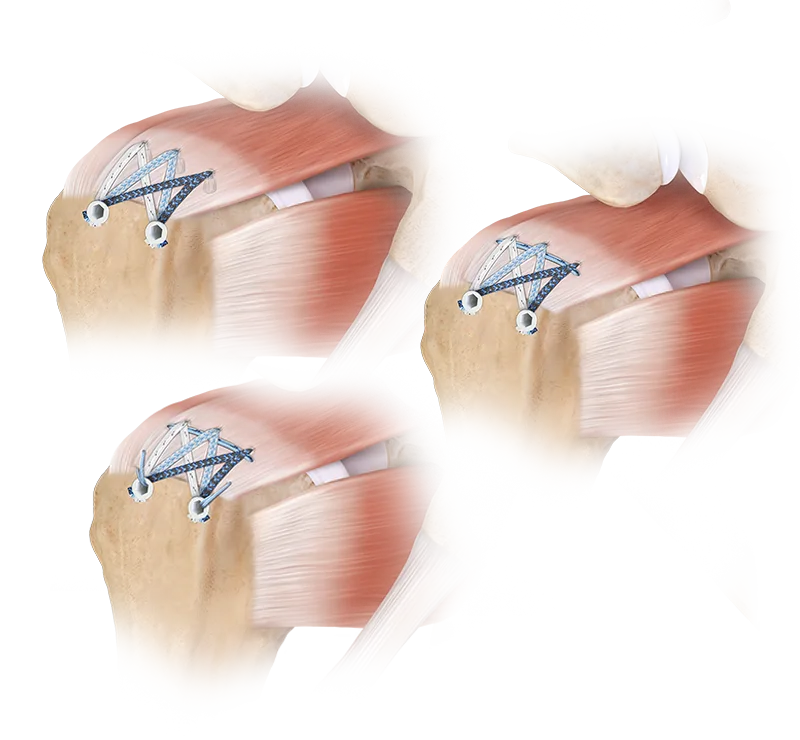
Rotator cuff repair surgery is a crucial procedure for treating rotator cuff tears, which affect the group of muscles and tendons that stabilize the shoulder joint and enable a wide range of motion. These tears, commonly resulting from injury, overuse, or degenerative changes, can cause significant shoulder pain, weakness, and loss of function. During rotator cuff repair, the torn tendons are reattached to the bone using sutures, anchors, or other fixation devices to restore the shoulder’s integrity. Following surgery, patients typically undergo a comprehensive rehabilitation program, including physical therapy, to regain strength, flexibility, and range of motion. This post-operative care is essential for a successful recovery, helping patients return to normal activities while reducing the risk of re-injury
Portland’s Leading Shoulder Impingement Surgeon
Arthroscopic shoulder surgery is a highly effective, minimally invasive procedure widely used to treat common shoulder conditions such as tendonitis, impingement, and bursitis. These conditions often arise from inflammation or irritation of the tendons, bursae, or surrounding structures, leading to shoulder pain, restricted movement, and discomfort. During arthroscopic surgery, a small camera (arthroscope) and specialized instruments are inserted through tiny incisions to diagnose and treat the underlying issues. For tendonitis, arthroscopy may involve debridement or smoothing of the inflamed tendon. In cases of shoulder impingement, the surgeon may remove bone spurs or other structures causing compression. For bursitis, the procedure typically includes the removal of the inflamed bursa. Arthroscopic surgery for the shoulder offers quicker recovery times, less post-operative pain, and reduced scarring compared to traditional open surgery, making it the preferred choice for many patients seeking relief from shoulder pain and mobility issues.

The Best Shoulder Instability Surgeon Near You
Treatment for shoulder dislocation involves both immediate care and long-term management to restore joint stability and prevent future occurrences. The initial step is reducing the dislocated shoulder, a procedure where a medical professional gently maneuvers the humeral head back into the socket. This may require sedation or anesthesia. After the shoulder is realigned, it is typically immobilized in a sling to allow the ligaments and tissues to heal. Following immobilization, physical therapy is essential to strengthen the rotator cuff muscles and improve the shoulder’s range of motion, which helps support the joint and minimize the risk of recurrent dislocations.
For cases of recurrent shoulder dislocation or significant ligament damage, arthroscopic surgery might be recommended to enhance joint stability. This minimally invasive procedure involves making small incisions to insert a camera and specialized instruments, allowing the surgeon to precisely repair or tighten the damaged ligaments while minimizing damage to surrounding tissues. Arthroscopic surgery for shoulder dislocation often results in faster recovery times, less post-operative pain, and quicker return to daily activities compared to traditional open surgery. It is especially beneficial for athletes and active individuals who face a higher risk of repeated dislocations. However, in more complex cases, open surgery may be required to fully address the issue and ensure optimal joint stability.
Portland’s Top Shoulder Replacement Surgeon
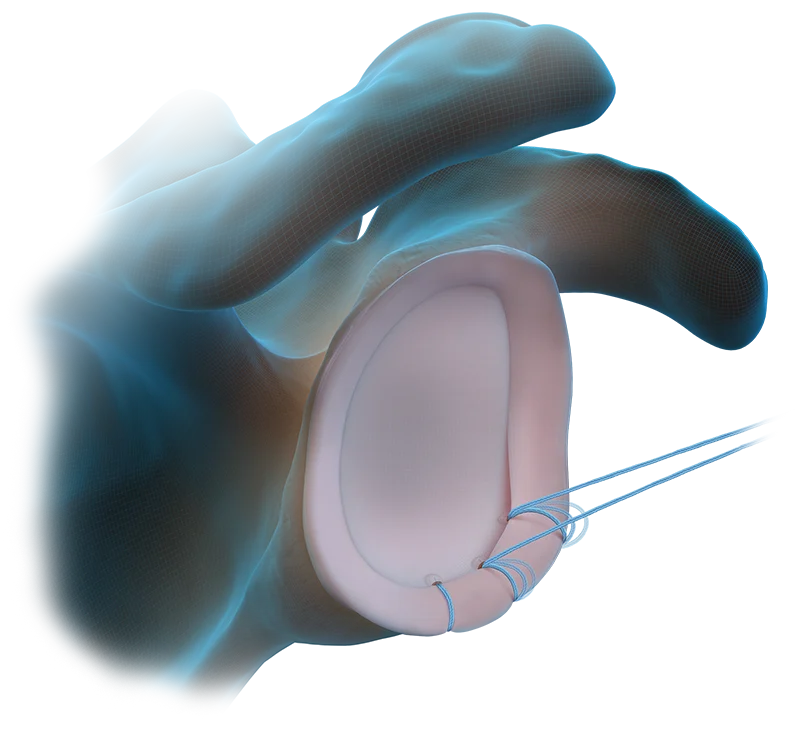
Shoulder replacement surgery, or shoulder arthroplasty, is a highly effective procedure for patients suffering from severe shoulder arthritis. Common types of arthritis, such as osteoarthritis and rheumatoid arthritis, often cause the cartilage in the shoulder joint to deteriorate, leading to pain, stiffness, and limited mobility. Shoulder replacement surgery addresses this issue by removing the damaged parts of the shoulder-namely, the humeral head (the ball) and the glenoid (the socket)-and replacing them with durable artificial components made from metal and plastic. This surgical approach aims to alleviate pain, restore shoulder function, and enhance the overall quality of life for patients who have not found relief through conservative treatments like medications, physical therapy, or injections.
Anatomic total shoulder arthroplasty is designed to replicate the natural anatomy of the shoulder joint, making it ideal for patients with arthritis or joint degeneration who still have an intact rotator cuff. This procedure involves replacing the damaged joint surfaces with a prosthesis that includes a metal ball and a plastic socket. The metal ball replaces the head of the humerus, while the plastic socket replaces the glenoid, the part of the shoulder blade. By restoring the normal alignment and movement mechanics of the shoulder, anatomic shoulder replacement aims to improve range of motion, reduce pain, and restore functional mobility. This approach is generally suited for patients with good rotator cuff function and relatively straightforward shoulder joint damage.
In contrast, reverse total shoulder arthroplasty is used when the rotator cuff muscles are severely damaged or torn, which can compromise the effectiveness of anatomic replacement. This procedure involves reversing the normal shoulder mechanics by placing a metal ball on the shoulder blade (glenoid) and a plastic socket on the end of the humerus. The reversed design changes the center of rotation of the shoulder joint, enhancing stability and leveraging the deltoid muscle to lift and move the arm. This modification helps compensate for the loss of rotator cuff function and is particularly beneficial for patients with severe rotator cuff tears or complex shoulder arthritis. Reverse total shoulder arthroplasty aims to improve arm function and alleviate pain in conditions where traditional anatomic replacement might not be effective.
Post-surgery, a structured physical therapy program is crucial for regaining strength and range of motion, with many patients experiencing significant pain relief and functional improvement.

Regenerative Medicine Specialist

Cutting-edge regenerative medicine, otherwise known as orthobiologics, is used for several types of shoulder conditions. These innovative therapies leverage biological substances to boost the body’s natural healing abilities.
Rthobiologics includes a broad spectrum of treatments, such as platelet-rich plasma (PRP), bone marrow aspirate concentrate (BMAC), micro-fragmented adipose tissue (MFAT) and shockwave therapy. These treatments are increasingly being used to address various orthopedic conditions, such as supporting natural healing, supporting tissue regeneration and reducing inflammation.
These orthobiologic treatments represent the forefront of non-surgical options for improving shoulder health and function, offering new hope for patients seeking relief from chronic shoulder conditions.
Frequently Asked Questions
How is a rotator cuff tear diagnosed?
Diagnosing a rotator cuff tear involves a multifaceted approach, with the physical examination playing a crucial role. The physical exam is often the initial and most critical step in diagnosing a rotator cuff tear. During this examination, your doctor will assess shoulder pain, range of motion, strength, and specific movement patterns. They may perform various tests to evaluate the presence of a rotator cuff tear and determine its severity. These tests can provide valuable insights into the function and condition of the shoulder muscles and tendons. While the physical exam is essential for identifying symptoms and narrowing down the potential causes of shoulder pain, imaging studies, such as an MRI, are used to confirm the diagnosis and assess the extent of the tear. An MRI provides detailed images of the soft tissues, allowing the physician to visualize the rotator cuff tendons and detect any tears, inflammation, or other abnormalities. However, it’s important to note that while MRIs are highly useful for confirmation and planning treatment, they do not replace the need for a thorough physical examination. Thus, a comprehensive approach combining both physical examination and MRI is crucial for accurate diagnosis and effective treatment planning for rotator cuff tears.
What non-surgical treatments are available for shoulder impingement?
Treatment for shoulder impingement typically starts with conservative approaches such as physical therapy and corticosteroid injections to reduce pain and improve function. However, cutting-edge treatments like Platelet-Rich Plasma (PRP) therapy are gaining recognition for their effectiveness in addressing more persistent cases and lack of side effects compared to steroid injections. PRP therapy involves extracting a small sample of the patient’s blood, concentrating the platelets, and injecting this solution into the shoulder joint. The platelets are rich in growth factors that promote healing and reduce inflammation in the affected area. By harnessing the body’s natural healing processes, PRP therapy can accelerate recovery and alleviate symptoms of shoulder impingement more effectively than traditional treatments alone. This innovative approach offers patients a promising option for relieving chronic pain and enhancing shoulder function.
When is shoulder replacement surgery necessary?*
Shoulder replacement surgery is usually considered for patients with severe shoulder arthritis or joint damage that has not responded to conservative treatments such as medications, physical therapy, or injections. The surgery involves replacing the damaged joint surfaces with artificial components to relieve pain and restore function. It is typically recommended when pain and stiffness significantly impair daily activities and quality of life.
What should I expect during recovery from shoulder surgery?
Recovery from shoulder surgery involves a structured rehabilitation process, including physical therapy to restore strength, flexibility, and range of motion. Patients can expect an initial period of immobilization to allow healing, followed by gradual physical therapy exercises to rebuild shoulder function. The recovery timeline can vary depending on the type of surgery performed and the individual’s overall health. Your doctor will provide specific guidelines and milestones to help ensure a successful recovery and return to normal activities.